Ever noticed that your blood glucose doesn’t always behave the same way after eating, even when you’ve had the same meal?
You’re not imagining it. What happens to blood glucose after a whole mix of factors, including digestion, hormones, activity, and timing, influences a meal.
Let’s take a look at what usually happens in people without diabetes, then how this can differ in Type 1 and Type 2 diabetes, and what you can do to spot patterns and manage post-meal spikes.
Contents
After a meal: What happens to blood glucose without diabetes?
What’s different in Type 1 diabetes?
What about Type 2 diabetes?
GI and GL: Why some foods raise blood glucose faster
Why the same meal can give different results
Insulin timing: Why 15 minutes can matter
Tips for managing post-meal glucose & spotting patterns
The bottom line
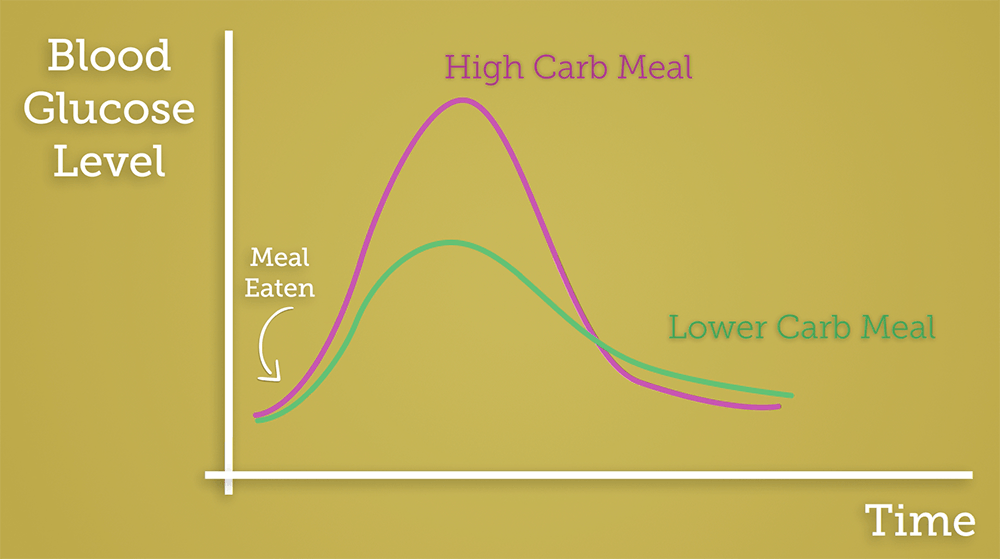
After a meal: What happens to blood glucose without diabetes?
When someone without diabetes eats a meal containing carbohydrates:
- Carbohydrates are broken down into glucose during digestion.
- Glucose enters the bloodstream, causing blood glucose levels to rise.
- The pancreas releases insulin, which helps glucose move from the blood into the body’s cells.
- Blood glucose levels usually peak within 1–2 hours, then return to baseline.
This process is tightly regulated. Insulin is released quickly and efficiently, preventing large spikes or prolonged highs.
What’s different in Type 1 diabetes?
In Type 1 diabetes, the body no longer produces insulin, so insulin must be given via injections or a pump.
After a meal:
- Carbohydrates still break down into glucose as normal.
- Blood glucose rises — but without insulin, it can keep rising.
- Mealtime insulin is needed to match the carbohydrate eaten.
This is where timing becomes really important. Rapid-acting insulin usually works best when taken around 15 minutes before eating (sometimes called pre-bolusing), so it’s already starting to work as glucose enters the bloodstream.
If insulin is taken too late:
- Glucose may spike quickly
- Levels may come down later, increasing the risk of hypos
What about Type 2 diabetes?
In Type 2 diabetes, insulin is still produced, but:
- The body doesn’t respond to it as effectively (insulin resistance).
- Insulin release may be slower or insufficient.
This can lead to:
- Higher and longer-lasting post-meal glucose rises.
- Blood glucose staying elevated for several hours.
Medication, meal composition, portion size and activity levels all influence what happens next, which is why responses can vary so much between people.
GI and GL: Why some foods raise blood glucose faster
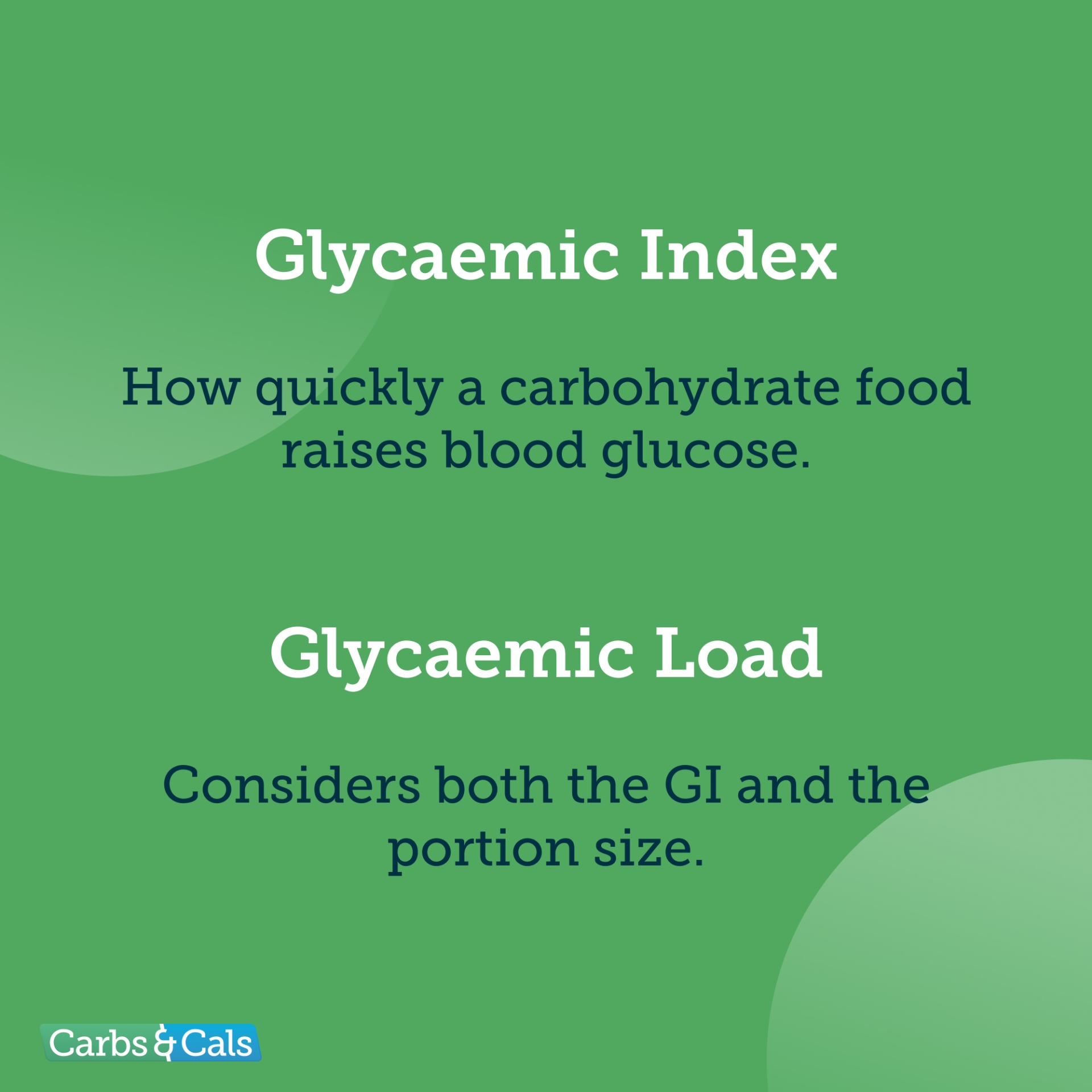
You might hear about Glycaemic Index (GI) and Glycaemic Load (GL) when talking about post-meal glucose.
- GI describes how quickly a carbohydrate food raises blood glucose.
- GL considers both the GI and the portion size, making it more practical.
For example:
- White bread → high GI, raises glucose quickly.
- Lentils → low GI, slower rise.
- A large portion of a low-GI food can still have a high GL.
Foods higher in fibre, fat or protein tend to slow digestion and lead to a more gradual rise. But this isn’t guaranteed.
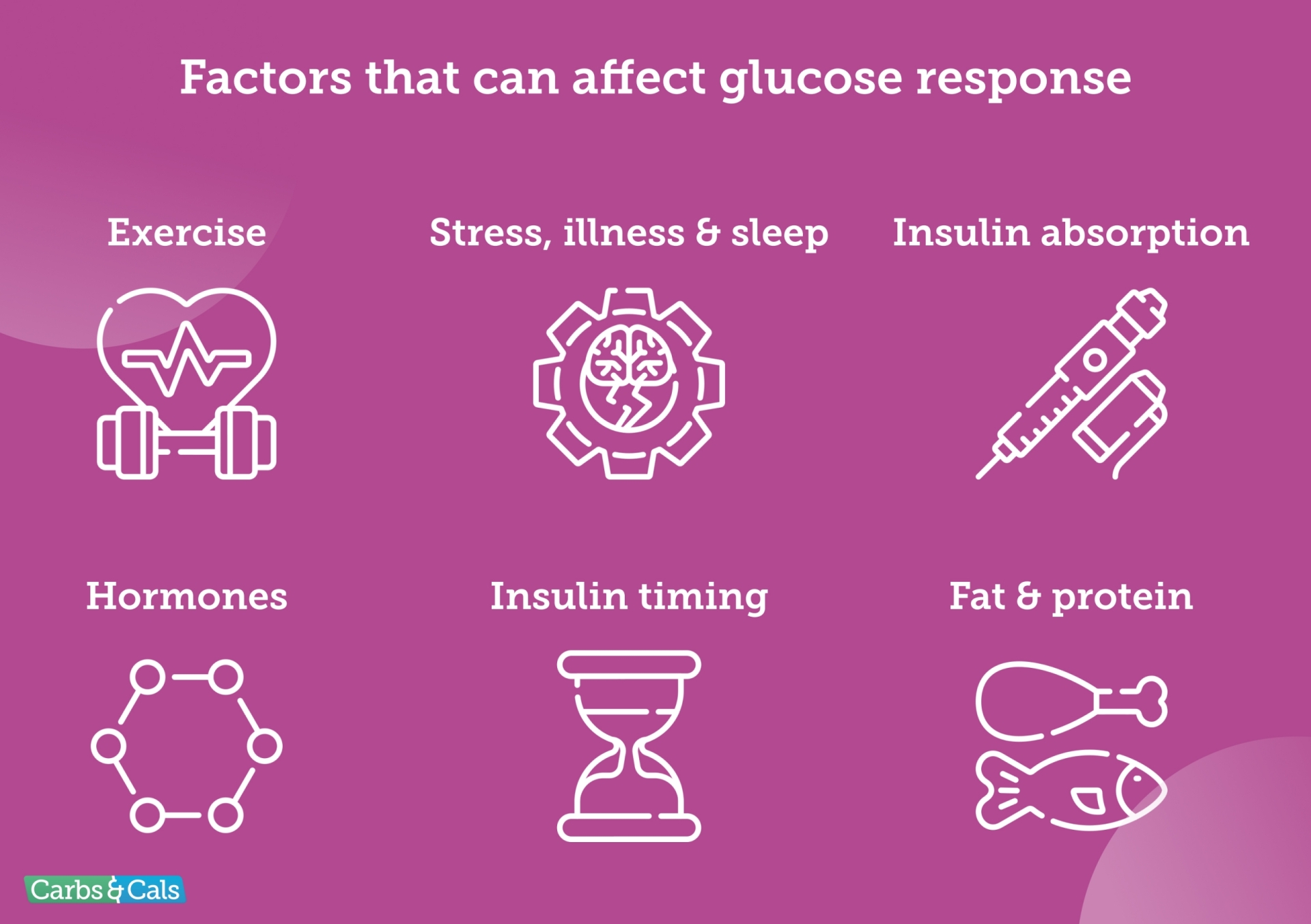
Why the same meal can give different results
One of the most frustrating things about diabetes management is that the same meal can cause different glucose responses on different days.
This can be due to:
- Exercise earlier in the day (or even the day before).
- Stress, illness or poor sleep.
- Insulin absorption (injection site, scar tissue, temperature).
- Hormones (especially in the morning or around menstrual cycles).
- Timing of insulin relative to the meal.
- Fat and protein content, which can delay glucose rises.
This variability is normal, and not a sign that you’re “doing it wrong”.
Insulin timing: Why 15 minutes can matter
For people using rapid-acting insulin, taking insulin around 15 minutes before eating can:
- Reduce post-meal spikes.
- Improve Time in Range.
- Better match insulin action to digestion.
That said, timing should always be individualised. This is something to review with your healthcare professional.
Tips for managing post-meal glucose & spotting patterns
Rather than aiming for perfection, focus on patterns over time.
1. Look at trends, not one-offs
A single high reading doesn’t tell the whole story. Repeated rises after similar meals or at a similar time of day are more meaningful.
2–4 hours post-meal is a good time to check whether blood glucose levels have returned to your usual range or stayed high.
2. Consider different causes
What other factors may be at play?
- Have you done physical activity that day, or even the day before?
- Have you had alcohol?
- Have you had a lot of stress or poor sleep?
These may all be one-off reasons for a change in your post-meal readings.
3. Consider timing, accuracy and medication
If you take insulin:
- Did you inject before or after eating?
- Have you taken other prescribed diabetes medication at the correct time and dose?
- If you carb count, were you accurate with the carb estimation?
- Have you had rapid-acting insulin in the last 2–4 hours that could cause insulin stacking?
4. Fat & protein
Was the meal high in:
- Fat (above 30 g)
- Protein (above 40 g)
Both can lead to a slower rise in blood glucose and, in some individuals, a greater insulin requirement later on.
If you feel these types of meals affect you, talk to your healthcare team about options for managing delayed post-meal rises.
5. Adjust one thing at a time
If making changes to portions or insulin doses based on patterns you’ve seen, it’s best to do this slowly and one change at a time.
Always talk with your healthcare team if you’re unsure how to adjust insulin doses or if you haven’t been trained through a structured education programme such as DAFNE.
The bottom line
After a meal, blood glucose rises for everyone. That’s normal physiology. What differs is how high, how fast, and how long it stays elevated.
Understanding:
- Food type (GI and GL).
- Insulin and other medication timing.
- Day-to-day variability.
- Other factors, such as the influence of exercise.
…can help you make sense of your numbers and focus on realistic, achievable improvements rather than chasing perfection.
Small tweaks, spotted through patterns, often make the biggest difference over time.
Want to Learn More?
Grab a Copy of Carb & Calorie Counter
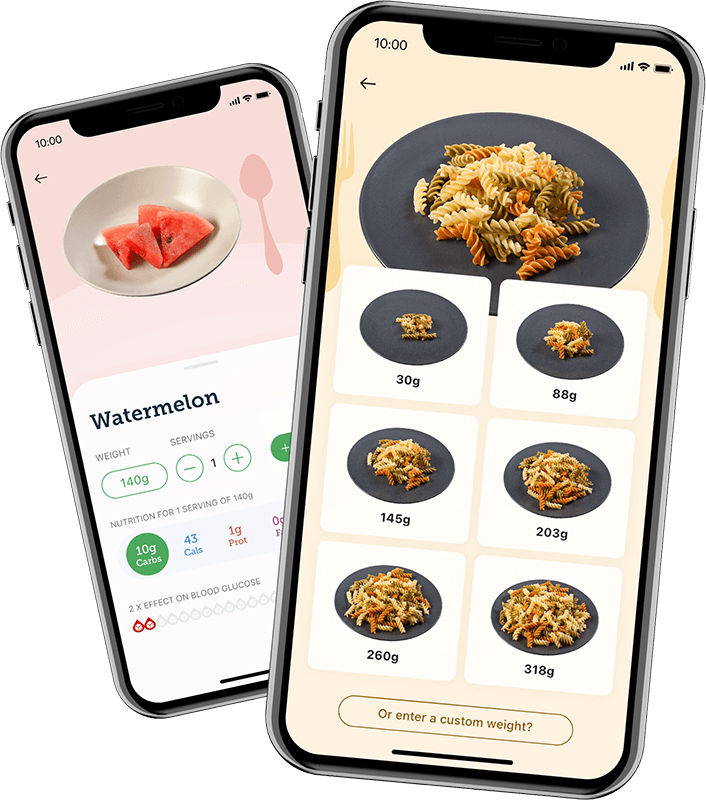
The multi-award-winning Carb & Calorie Counter book is your definitive, expert-approved guide to carb and calorie counting.
- Over 1700+ high-quality food photos
- Up to six portion sizes per food
- At-a-glance carbs and key nutrients
- The Original #1 Bestseller
With the “Carb-Counting Bible”, a single flick of the page is all you need to plan nutritious, carb-counted meals.
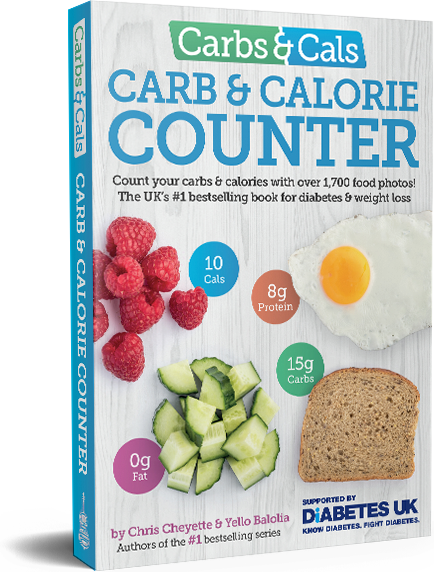

Contains hundreds of food photos that makes carb counting easy!
Sign up to the Carbs & Cals mailing list
Want to learn more about carb counting and the role of food in managing your health? Sign up to our mailing list!